Introduction
About "Fallen" and "Weak" Bladders: What can be done.
Women sometimes refer to bladder issues as a "fallen" or "weak" bladder. Likely what they're describing is some type of pelvic organ prolapse where the bladder is no longer in its original position. Symptoms often include urinary incontinence and pelvic pain. We can help with these conditions.
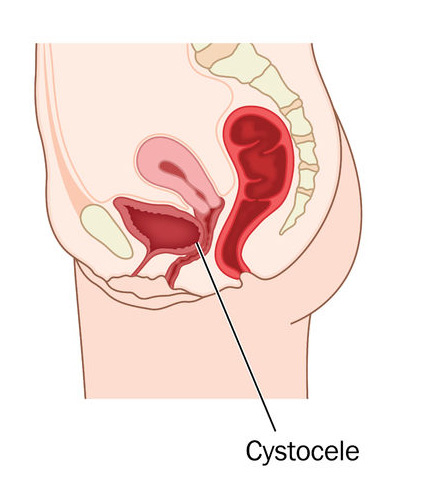
Cystocele:
Fallen or Dropped Bladder
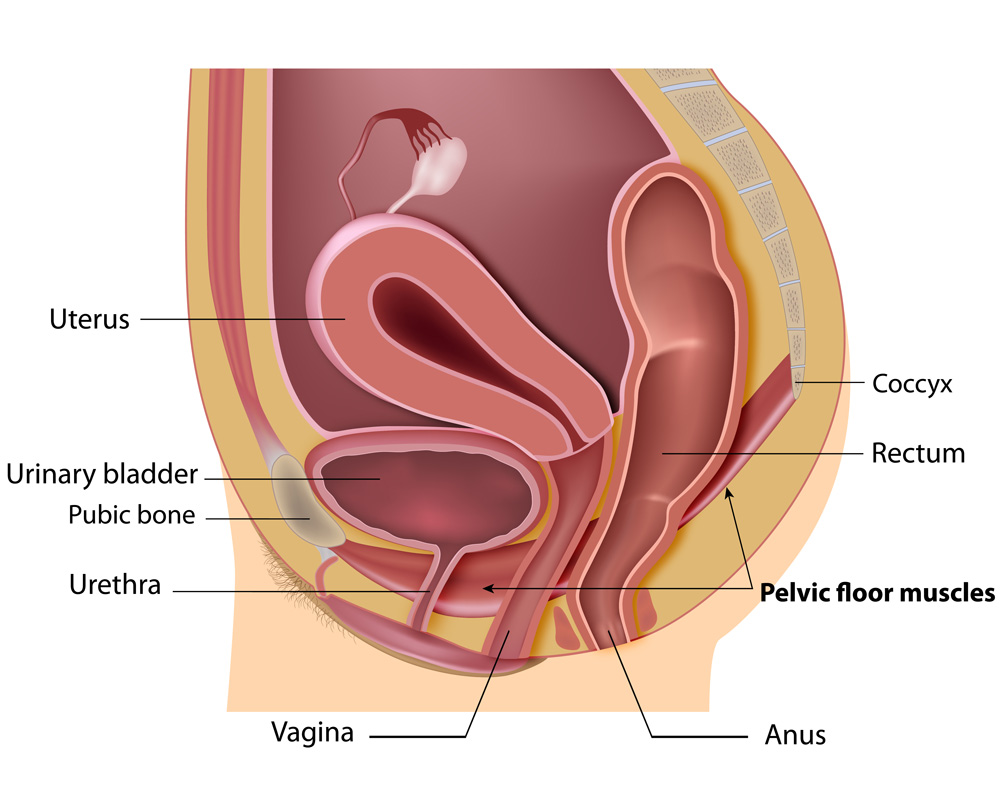
Cystocele (or bladder prolapse) is a condition in women where the bladder is no longer in its normal position. It "drops" and bulges into the vagina when the supportive tissues between the bladder and vagina weaken and stretch.
What causes a cystocele? A dropped bladder – or cystocele – may result from damage to the muscles and tissues that that make up the pelvic floor. Damage to or weakening of the pelvic structure can occur after vaginal childbirth. In addition, movements and conditions that strain or increase pressure can also cause the bladder's position to change. The chances of a cystocele increase with age and after menopause.
Symptoms of a Cystocele:
Fallen or Dropped Bladder
Symptoms of a cystocele may include a vaginal bulge, the feeling that something is falling out of the vagina, the sensation of pelvic heaviness or fullness, feelings of incomplete urination and stress urinary incontinence – the involuntary leaking of urine when you cough, sneeze, laugh, or engage in physical activity.
Treatment for a Fallen or Dropped Bladder (Cystocele)
We always begin with an accurate diagnosis. We use rehabilitative and curative care plans that are attentive to our patients' emotional, educational and physical needs. Where surgery is required, your care plan may include both pre- and post- operative physical therapy to rehabilitate your pelvic function.
There are a number of ways to treat this condition. We'll work with you to determine what course of action is the best one for you. Don't give up or be embarrassed! Remember, many women have this condition and have been successfully treated at every age.
If surgery is necessary to restore your health, you're in good hands. Dr. Melvin Ashford, the founder of Minnesota Women's Care, is board-certified in Urogynecology & Reconstructive Pelvic Surgery (URPS). (Formerly Female Pelvic Medicine and Reconstructive Surgery – FPMRS.) This means he has the training and experience for the specific diagnosis and surgical repair of pelvic organ prolapse and other pelvic organ disorders.
Surgical Repair of Cystocele or "Fallen" Bladder
This type of repair often brings up use of mesh - a controversial topic for some. Dr. Ashford has answered questions in the past about mesh and the use of it for repairing pelvic organ prolapses such as cystocele.
Through the years, many women have experienced favorable results with the use of mesh to repair pelvic organ prolapses. There are options to repair these pelvic floor disorders without the use of mesh.
Dr. Ashford and our surgical team has the training and experience to address these issues and make the best surgical correction. Talk with us. We can help.